Recently, I decided to purchase a continuous glucose monitor (CGM), even though I don't have a diabetes diagnosis. My goal was to gain a deeper understanding of how my diet might affect my health. CGMs provide real-time feedback on blood glucose levels, which intrigued me, especially given the growing popularity of GLP-1 drugs like Ozempic. Ozempic, the brand name for semaglutide, is primarily used to treat type 2 diabetes but has also gained attention for its role in weight management for individuals with obesity or overweight.
Scientists are raising concerns about the rising rates of cancer in the U.S., especially among younger populations. The American Cancer Society (ACS) highlights that obesity is a significant risk factor for at least 13 types of cancer, including breast, colon, and thyroid cancers. According to the ACS, these cancers may be caused by several mechanisms, such as hormonal changes (e.g., increased estrogen levels in obese women), insulin resistance, and chronic inflammation.
Some attribute the rise in cosmetic use among younger people to the influence of social media, which may also contribute to the increase in cancer rates. Many cosmetics contain chemicals that could pose health risks. For instance, sunscreens often include more than 50 chemical ingredients, yet manufacturers are not required to list all of them on the label.
While there is at least one other CGM available to consumers without a prescription, I purchased the Dexcom G7 CGM, which the Food and Drug Administration (FDA) approved for use in non-diabetic consumers in 2022. The monitor cost $89 for the first month of use, and it took a few days to arrive. The package included two wearable patches, each about one inch in diameter, which are applied to the back of the upper arm and stay in place for about two weeks. Although I’m usually very sensitive to things on my body— for example, I can’t wear earrings while I sleep—I barely notice the monitor. It was completely painless to apply, despite the applicator looking a bit intimidating (see photo below).
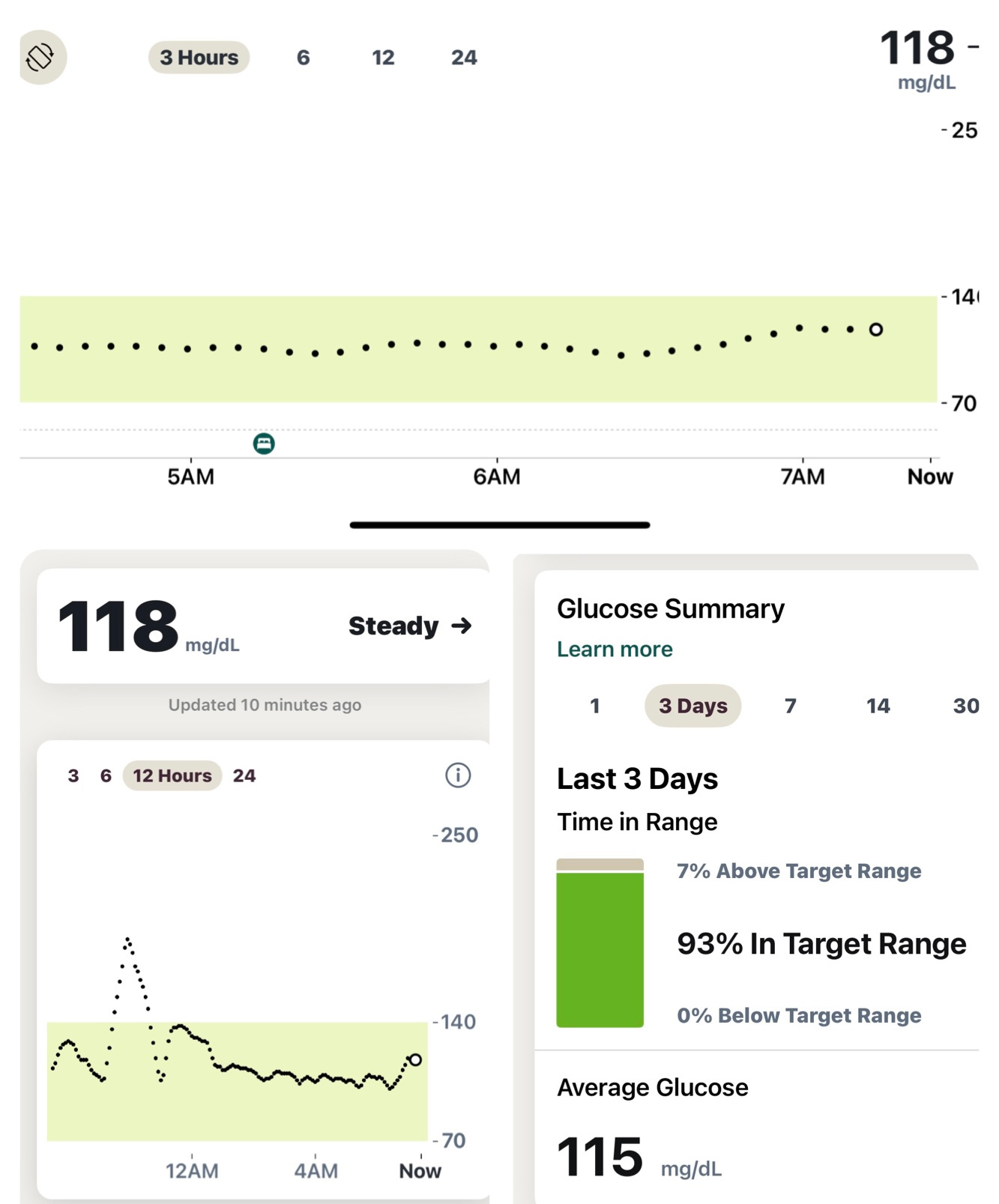
The monitor connects to a mobile app on my smartphone (see photo). I use an iPhone, and the app also syncs with the Health app, providing additional insights such as my glucose levels while I sleep. All of this data can be easily shared with my physician.
I’ve been using the monitor for less than a week, but I’m already learning valuable insights about how diet and exercise affect my glucose levels. For instance, I discovered that eating white basmati rice causes my blood glucose to spike outside my target range, while brown rice does not. Interestingly, dark chocolate without added sugar doesn’t cause any spikes. Additionally, my water intake—particularly having a glass before my first cup of coffee and throughout the day—seems to help stabilize my glucose levels. However, it's important to remember that individual responses can vary, so it's always a good idea to discuss any concerns with your physician.
Overall, using the CGM has been an eye-opening experience, providing me with real-time insights into how my lifestyle choices impact my glucose levels. For example, I discovered that just 15 minutes on the rowing machine significantly moderates my glucose levels, highlighting the importance of even short bursts of exercise. While I’ve learned a lot in just a short time, I recognize that managing blood glucose is a highly individual process. This experience has reinforced the value of personalized health monitoring and the importance of working with a healthcare provider to make informed decisions. I look forward to continuing to track my health and learning more about how small changes in my diet and habits can lead to better overall well-being.
Mindi Messmer, MS, PG, CG is an environmental and public health scientist and author of Female Disruptors: Stories of Mighty Female Scientists. The book is available on Amazon, Barnes & Noble and through your local bookstore.